Heat and destroy
With thanks to the generous support of the Worldwide Universities Network Research Mobility Program, I was able to visit collaborators at the picturesque University of Western Australia in Perth. The UWA physics department has one of the few research groups with a specific focus on biomagnetism. The aim of the research project was to try to improve techniques for magnetic hyperthermia, an experimental procedure for treating tumours.
Magnetic hyperthermia - the physics
If you have read any of my other research blog posts, you’ll know that we’re going to start with magnetic nanoparticles. They are not as advanced as they sound; a magnetic nanoparticle is a small particle of magnetic material (like iron or FeO3 for the chemistry buffs) around 0.00000001m in diameter. They are so small, in fact, that it can be difficult to determine their shape even by use of a microscope.
Many people will know - or will have experienced - magnetic resonance imaging. Otherwise known as an MRI scan. The imaging relies on a patient being placed into a magnetic field and using a detector to record the response of the hydrogen atoms present in the body. The procedure produces very high quality images and importantly is safe for patients because the magnetic field is not harmful to the human body.
In magnetic hyperthermia, a patient is put into a magnetic field in much the same way. The difference is that we must first introduce magnetic nanoparticles into the target area (i.e. the tumour). The magnetic field can then interact with the particles in a way that generates heat.
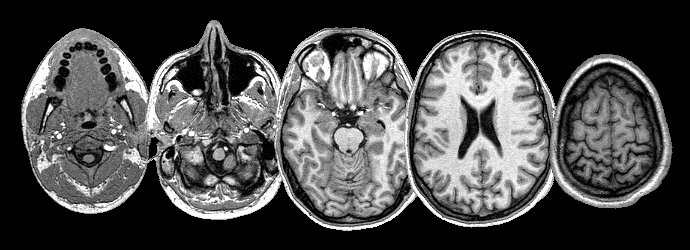 Magnetic resonance imaging (MRI) is a widely used diagnostic technique and a breakthrough in medical technology.
Magnetic resonance imaging (MRI) is a widely used diagnostic technique and a breakthrough in medical technology.
Targeting Tumours
Hence why we call the technique hyperthermia: hyper the Greek for above/excess and thermia for heat, literally to overheat. Using magnetic hyperthermia we are able to heat tumours to cytoxic temperatures - in other words, heat them enough to cause cell damage.
Fortunately tumour tissue struggles to survive at temperatures that are safe for healthy tissue, which means that we can treat tumours without harming the patient.
Our work
At the biomagnetism group at UWA we were interested in knowing whether placing patients in different types of magnetic field would make the procedure more effective, so that we could answer questions such as: ‘what is the best type of magnetic field to use?’ and ‘how would poor quality equipment affect the effectiveness of the heating?’.
The results of the work were interesting and will be coming soon in a future blog post.
The future of cancer treatment?
Magnetic hyperthermia is still in its infancy and has a long way to go before reaching full-scale clinical trials. Whilst there have been some human trials, which have successfully extended life for patients with pancreatic cancer, there is a chasm of medical research to be done before magnetic hyperthermia can become a standard procedure. Whilst the physicists and engineers are busy optimising particle types and magnetic fields, chemists and medics devising methods for administering magnetic particles to the tumour accurately.